The long-awaited coronavirus vaccine is finally here. With our healthcare providers and other staff members being vaccinated recently, including the staff at Capital Rheumatology and myself, the excitement is growing amongst our patients to receive the vaccine themselves. Many of our patients with rheumatoid arthritis, lupus, and other autoimmune diseases have professions in the healthcare field like nurses, physical therapists, or social workers. Additionally, last week North Carolina moved towards phase 2, which includes patients above the age of 65. Thus, more and more people are asking if and when it is okay to receive the vaccine.
First and foremost, despite the good news, everyone must continue to follow safety precautions: wear a mask, maintain physical distance, practice proper handwashing, and clean high-touch surfaces.
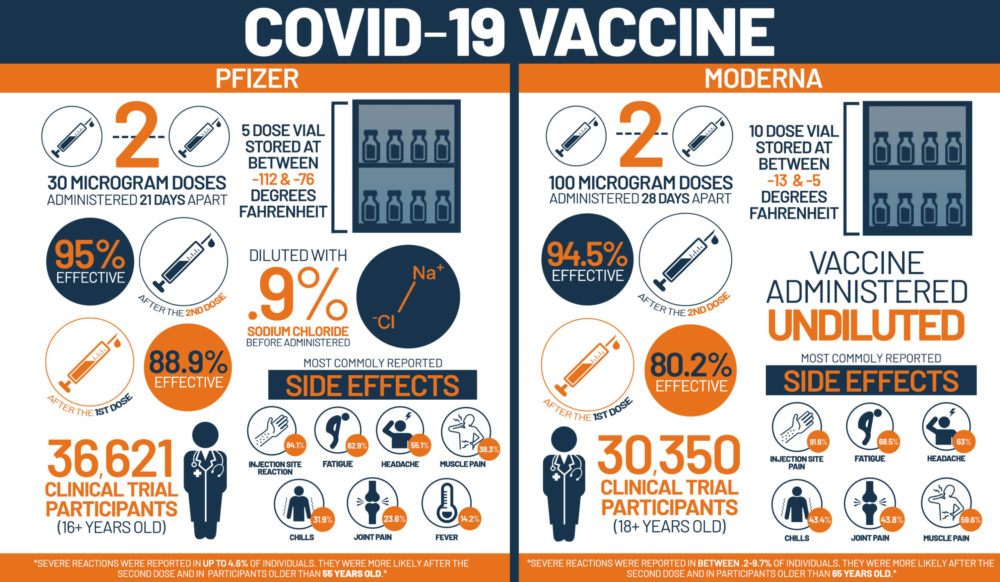
Next, we advise patients to avoid live vaccinations if they are on biologics. Fortunately, both approved vaccines do not use any live virus to create antibodies. The two vaccines available in North Carolina are from Pfizer and Moderna Therapeutics. They are provided as 2 injections either 3 or 4 weeks apart, respectively. The common side effects reported are those with most vaccinations such as fatigue, headache, sore arm, or fever. The data for both vaccines show they are equally effective and safe for most adults. The phase 3 clinical trials for this vaccine had much higher participants than normal, which provided a breadth of knowledge for many different types of patients and safety signals.
QUESTIONS & ANSWERS
I have an autoimmune condition. Should I be vaccinated?
Yes, it has been shown that people with autoimmune disease are at a higher risk of severe illness from COVID-19.
What about my medications? Is it best to continue these treatments?
The American College of Rheumatology has maintained guidance to continue your medications unless you develop an infection of any sort. It is advised that not treating your chronic illness will lead to a prolonged recovery period and increased risk of complications from COVID-19 infection.
Should I continue my therapy before and after vaccination?
We do not have data providing recommendations to hold your treatment with regards to the vaccination. There are ongoing studies and should receive more information in the coming months.
Do I still need to have the vaccine if I have already had the COVID-19 infection?
After recovering from an infection you can have multiple outcomes. Some persons may develop weak immunity, or it may wane within months. Thus, it is encouraged that you receive the vaccine to strengthen your protection as the benefits far outweigh the risks of the vaccine or contracting COVID-19 infection.
Does the vaccine cover for the new strain?
As we have seen on the news recently, a new strain of the virus is spreading. This has not had any effect on the vaccine which will continue to protect against this new strain. However, this strain is much more transmissible between people. Thus, any protection with the vaccination would be considered beneficial.
Where can I get vaccinated?
The North Carolina Department of Health and Human Services has clear guidelines on who will get the vaccine based on their risk for developing COVID-19. After discussing with your rheumatologists and/or primary care provider, you can schedule an appointment through the resources provided on the NCDHHS website. The large hospital care systems in our area are also scheduling patients. Sign in to your Duke/UNC/Wakemed myChart accounts (patient portal) to see if you are eligible. You can also schedule through the UNC COVID-19 Vaccine website (yourshot.org).
Additional Information
The information is ever-evolving and we will continue to help you understand it. For the latest guidance about COVID-19, CDC.gov is an excellent and reliable resource. We are also here to answer any questions and allay any concerns.